Om's Food Hygiene Intervention - December 2013

What a busy few months!
After the completion of the food hygiene intervention trial in early September, four major activities were took place through to December:
- Multi-sector policy analysis
- Measurement of trial outcomes
- Trial compliance measurement
- Dissemination of findings at national level
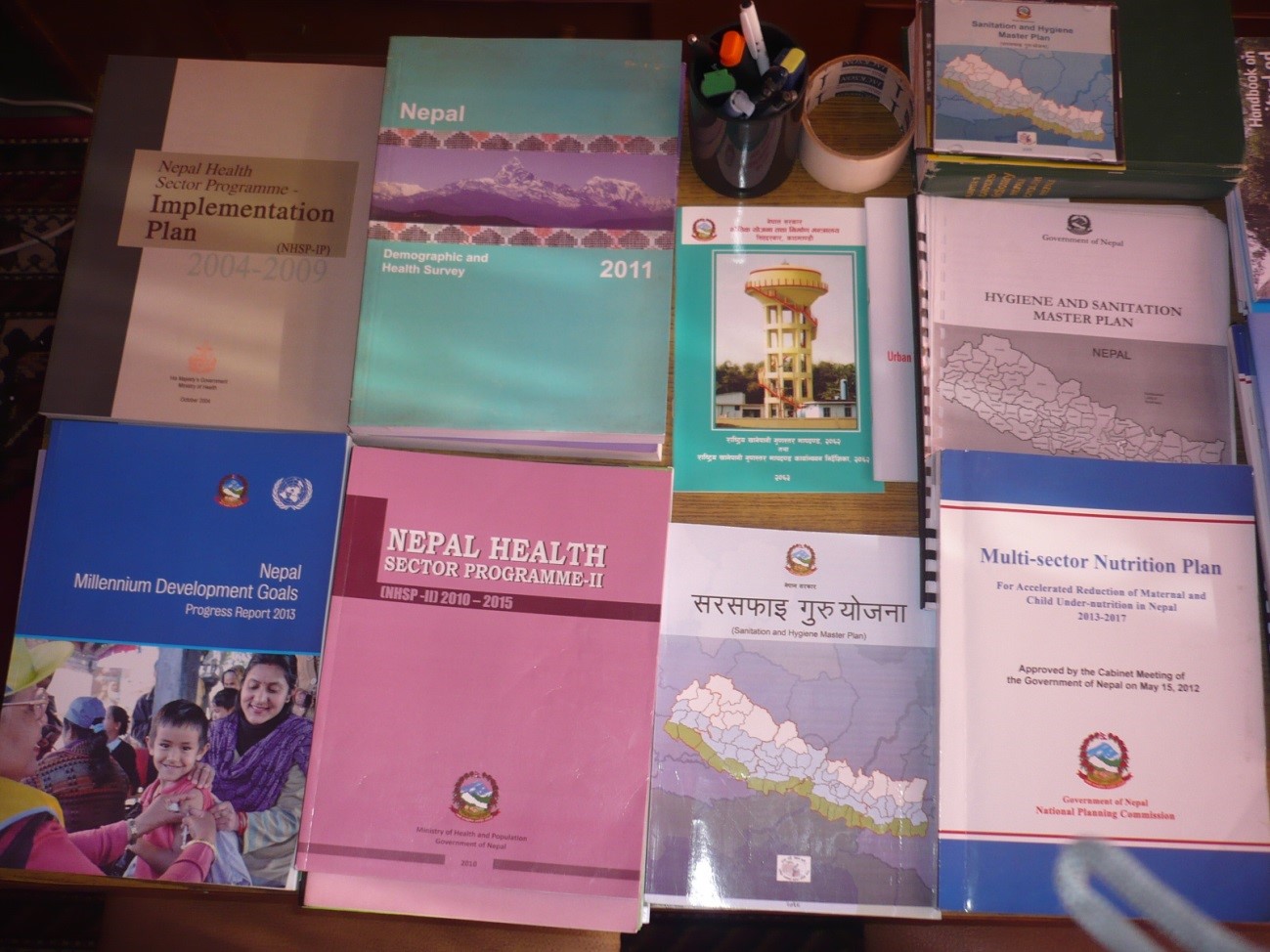
Multi-sector policy analysis: To explore how a food hygiene intervention might be integrated into sector strategies and programmes for nutrition, health, WASH, food technology & quality control in Nepal, I reviewed various government sector policies, strategies, and programme guidelines. Any policies, strategies, programme documents within the timeframe of 1990-2013 were included for the review, which I carried out mid September-mid October 2012. Altogether nine key documents were reviewed for health sector including the “Nepal Health Sector Programme-II (2010-2015)”; three key nutrition sector documents, including the ‘Multi-Sector Nutrition Plan (2013-2017)”; six key WASH document, including the “Sanitation and Hygiene Master Plan (2011); and four key food technology & quality control documents, including the “Food Act and Minimum Quality & Quality Standard for Food”.
Policy and programme adherence to food hygiene and its programmatic gaps, institutional responsibilities and barriers, as well as possible ways and opportunities for integration were highlighted. In addition, to triangulate the desk review findings and identify current practices on implementation of food hygiene-related programme/activities, key informant interviews were conducted with 12 policy and programme development professionals. Key informants included the sectoral ministry/department and key donor/INGO personnel directly engaged in the relevant areas. II.
Measurement of trial outcomes: The trial outcomes were only measured 45 days after completion of the intervention. The food hygiene behaviours of mothers (with a child aged 6-59months) were observed, and food, milk and water samples were tested to assess the level of contamination (microbes). Period prevalence of diarrhoea among young children (6-59months) was recorded from both the “intervention” and “control” arms.
Structured observation of mothers’ “food hygiene behaviours”: To observe behaviours, 25 food hygiene observers (FHOs) were recruited, given skilled and field based training, and mobilized accordingly. In each house, the observations took place from 1 to 5pm, when the behaviours of interest were likely to be seen. Observers paid particular attention to key food hygiene behaviours and recorded them accordingly. To minimize the effect of the presence of the observers, participant mothers were told that this was a daily routine assessment of mothers. Observers were only allowed to use a notebook, and were requested to talk about recent rituals/events in the village and minimize gossiping in the mother’s house to provide focused attention on the mothers’ behaviours. Observers had to fill the checklist immediately after their return home from the field, using notebook details, and submit the form the very next day to our field staff. Within 12 days, all mothers’ behaviours from eight clusters from both study arms (120 householder in intervention group and 117 households in control group) were observed and a day review meeting with observers was conducted to document their learning.






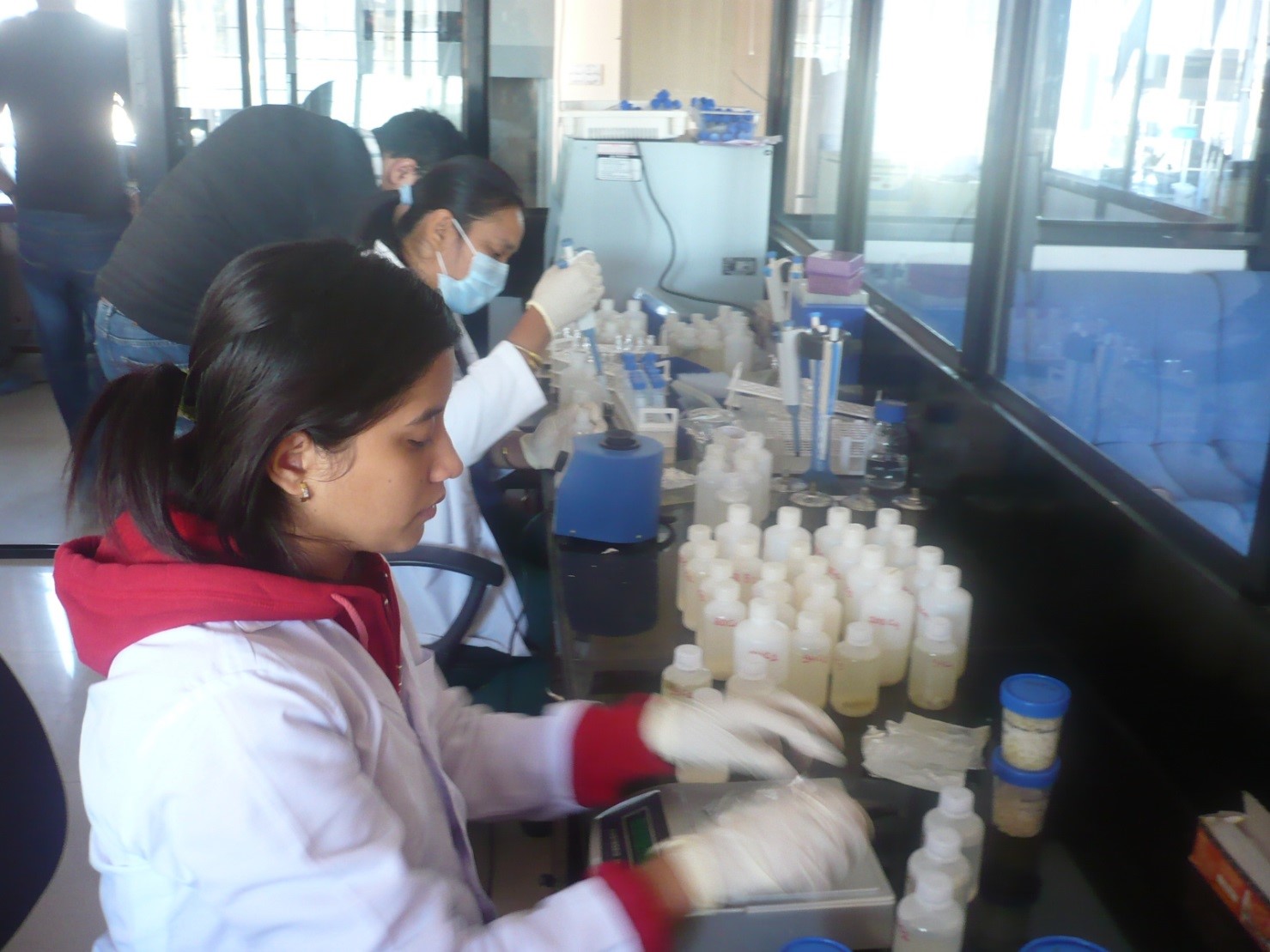
Microbe assessment in food, water and milk: Like with the baseline, altogether 248 food samples, 80 water samples and 45 milk samples were collected from the eight clusters (from both the intervention and control groups), using a standard protocol. The collected samples were then transported into a lab, maintaining an adequate temperature (<60C), and samples were processed, homogenized, inoculated, incubated. Results were then interpreted using standard operating guidelines. 3M PetriFilm for food & milk and membrane filter & Hi-chrome coliform media were used for water samples test. From all the samples, the total number of coliforms and E.coli were (CFU/gram in food and CFU/100ml in water) quantified.

Diarrhoea period prevalence measurement: To measure the effect of the intervention on diarrhoea prevalence, all mothers from eight clusters with a child aged 6-59 months were asked if their child had had diarrhoea in the last 7 days. If yes, then the WHO definition was used to confirm the case i.e. ‘the passage of 3 or more loose or liquid stools per day or more frequently than is normal for the individuals’.

Trial compliance measurement: To ascertain whether or not the intervention reached the intended target groups and to assess the exposure and reach of the intervention, the compliance measurement was done in both the intervention and control arms. In this exercise, mothers were asked whether they have heard of, attended or followed campaign events/visits.This measurement was extremely useful in assessing whether there was any cross-contamination during the trial period. In addition, mothers from only the intervention group were asked to rank the behaviours taught in the trial using an illustration according to how easy or difficult they were to perform. Through focus group discussions, we had also tried to capture the key motivational factors/tools/approach for mothers to change and adopt key food hygiene behaviours. We also asked mothers questions that helped us explore whether change in behaviours over time has any role in changing social norms.


Dissemination of the findings at national level: A national dissemination workshop was organized in Kathmandu on 10th December 2013 after successful accomplishment of the trial. Here, I presented and shared the full findings obtained from formative research, as well as the preliminary findings of the food hygiene intervention trial and policy analysis. The outcomes of the trial were well received and there was lots of positive feedback.
A 19 minute video documentary of the trial was also shared during the event.
In order to demonstrate and provide an opportunity to have a look at the tools/materials used for the programme, a display stall was set-up. More than 60 distinguished guests, including colleagues from the Prime Minister Office, National Planning Commission, the health, WASH, nutrition, agriculture, education, and food technology sectors, as well as donors and NGOs attended the workshop.


Access a visual representation of the trial on this useful poster.
